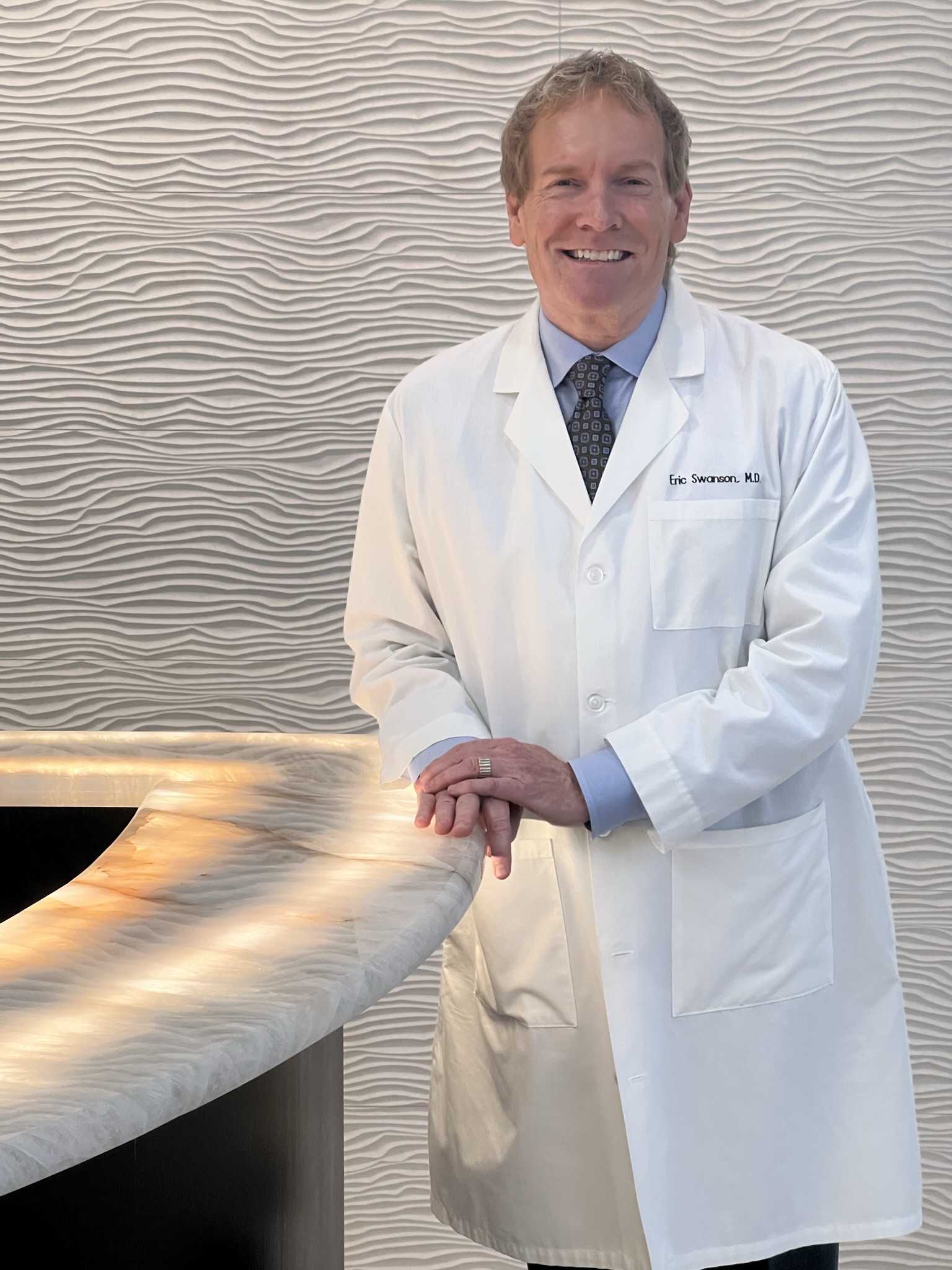
Dr. Eric Swanson, a board-certified plastic surgeon in private practice in Leawood, Kansas, is an advocate for the application of the scientific method to cosmetic surgery, an approach known as evidence-based medicine.
Dr. Swanson is a frequent presenter and invited faculty member at national and international meetings. Dr. Swanson has authored over 200 publications in peer-reviewed plastic surgery journals.